
Picture this: you’re a new parent, and your little one seems fussy after every feeding. You might wonder, “Could my baby actually be allergic to my breast milk?” It’s a question that worries many parents, and you’re not alone in asking it!
Here’s the surprising truth: babies can’t be allergic to breast milk itself. However, they can react to foods that mom eats, which then pass through her milk to the baby.
Think of it like a food delivery service, sometimes the “order” doesn’t agree with the customer!
A mother’s breast milk changes flavor based on what she eats; babies can taste garlic, vanilla, and even spices!
Ready to become a baby allergy detective?
Can Babies Truly Be Allergic to Breast Milk?
The simple answer is no, babies cannot develop a true infant milk allergy to their mother’s breast milk itself.
What many parents mistake for breast milk allergies are reactions to food proteins that pass through the mother’s diet into her milk.
When a baby shows signs of breast milk protein intolerance, they’re typically reacting to cow’s milk proteins, soy, eggs, or other allergens that the mom consumed.
Exclusive breastfeeding and allergies can still occur, but the culprit is always something in the milk, not the milk itself.
True allergies to human breast milk are medically impossible since babies’ immune systems are designed to accept their mother’s milk as the perfect food source.
Signs and Symptoms to Watch For: Breast Milk Allergies

When your baby seems uncomfortable after nursing, it’s natural to wonder if they’re having an allergic reaction.
These symptoms might look scary, but they’re usually your baby’s way of responding to something in your diet rather than your actual breast milk.
Here are common baby symptoms of milk allergy that parents often confuse with breast milk allergies:
- Rash or eczema – Red, bumpy skin patches that appear after feeding sessions, but are usually caused by food proteins in mom’s diet.
- Vomiting or diarrhea – Frequent spit-up or loose stools that seem linked to nursing but typically indicate sensitivity to something mom ate.
- Blood in stool – Streaks of blood in the baby’s diaper signal inflammation from food proteins passing through breast milk.
- Fussiness, colic-like behavior – Extended crying, gas, and irritability after feeds that parents mistake for breastfeeding allergy symptoms but stem from dietary triggers.
Remember, these symptoms don’t mean you should stop breastfeeding; they’re your baby’s way of telling you something in your diet might need adjusting. Keep a food diary and work with your pediatrician to identify the real cause of your little one’s discomfort.
What Causes Allergic Reactions in Breastfed Babies?
When your baby seems fussy or uncomfortable after nursing, the real troublemaker is usually hiding in your last meal or snack. Your breast milk acts like a delivery service, carrying proteins from foods you eat directly to your little one’s sensitive system.
- Dairy Products: Cow’s milk proteins from cheese, yogurt, ice cream, and milk are the top culprits for causing reactions in breastfed babies.
- Eggs: Whether scrambled, baked into cookies, or hidden in mayonnaise, egg proteins can pass through breast milk and trigger sensitivities.
- Soy Foods: Tofu, soy milk, soy sauce, and many processed foods contain soy proteins that some babies simply can’t handle yet.
- Nuts and Peanuts: Tree nuts and peanuts are potent allergens that can travel through breast milk and cause reactions in sensitive infants.
- Wheat and Gluten: Bread, pasta, cereals, and other wheat-containing foods might bother babies who have gluten sensitivities.
The good news is that most babies outgrow these food sensitivities as their digestive systems mature and strengthen.
With some detective work and your pediatrician’s guidance, you can identify what’s bothering your baby and continue to provide the best nutrition possible.
Food Allergy vs. Sensitivity vs. Lactose Intolerance
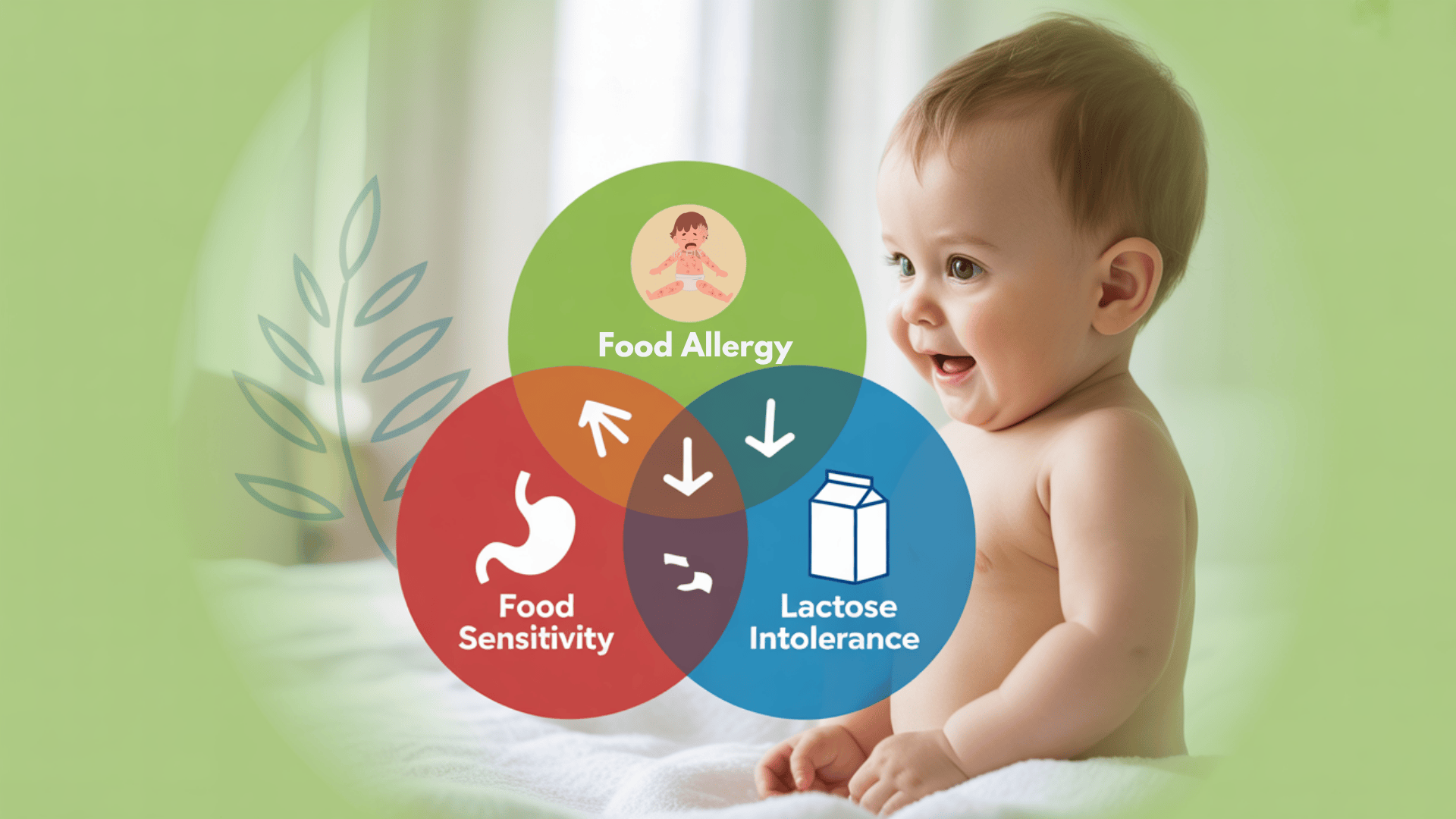
Not all baby reactions are created equal, and knowing the difference can save you from unnecessary worry!
When your little one seems uncomfortable after feeding, it helps to understand whether you’re dealing with a true allergy, a food sensitivity, or something else entirely.
| TYPE | CAUSE | SYMPTOMS | IMMUNE INVOLVEMENT | COMMON in BREASTFED BABIES? |
|---|---|---|---|---|
| Food Allergy | Immune reaction to food proteins | Rash, hives, vomiting, and blood in the stool | Yes | Rare |
| Food Sensitivity | Digestive response to certain foods | Gas, fussiness, mild eczema | No | Fairly common |
| Lactose Intolerance | Inability to digest milk sugar | Bloating, diarrhea, and stomach pain | No | Scarce under 6 months |
Understanding these differences helps you stay calm and make better decisions about your baby’s care. Remember, most issues resolve on their own as your baby’s digestive system develops and strengthens over time.
Treating Milk Allergies in Breastfed Babies

Here’s how to support your baby’s health through smart dietary changes, formula options, and gut-friendly strategies.
1. Dietary Changes for the Breastfeeding Mother
Dietary Changes for the Breastfeeding Mother: Start an elimination diet by removing dairy for 2-4 weeks, then soy if needed.
Include calcium-rich foods, such as leafy greens and fortified plant-based milks, in your non-dairy, breastfeeding diet; track baby’s symptoms to identify potential triggers.
2. Breastfeeding vs. Switching to Hypoallergenic Formula
Breastfeeding vs. Switching to Hypoallergenic Formula. A breastfeeding baby with a milk allergy usually requires dietary changes.
Hypoallergenic formula options, such as Nutramigen or Neocate, may be necessary for severe cases. Always consult your pediatrician first.
3. Probiotics and Gut Health
Probiotics and Gut Health: Probiotics, such as those containing Lactobacillus rhamnosus GG, may help reduce allergic responses by supporting gut health.
These can be given to mom or baby under medical guidance to help manage eczema and digestive symptoms.
4. Gradual Reintroduction Plan
Gradual Reintroduction Plan. After symptoms improve, doctors may suggest slowly reintroducing foods to test tolerance.
This helps identify specific triggers without long-term diet restrictions under medical supervision.
5. Nutritional Support for Mom
Nutritional Support for Mom Supplement with calcium, vitamin D, and omega-3 fatty acids when eliminating multiple foods.
Work with a dietitian to prevent deficiencies that could affect milk quality and your health.
6. Skin Care for Allergy-Related Eczema
Skin Care for Allergy-Related Eczema: Use hypoallergenic moisturizers, oatmeal baths, and gentle detergents to soothe irritated skin.
Keep baby well-moisturized and avoid harsh chemicals that worsen symptoms.
Myth vs. Reality: Separating Facts from Fiction
With so much conflicting information online, it’s easy for new parents to get confused about breast milk allergies. Let’s clear up some common misconceptions and give you the real facts you need.
Myth 1: Babies can be allergic to their mother’s breast milk
Reality: Babies react to proteins from the mother’s diet, not breast milk itself
Myth 2: Green poop means the baby is allergic to breast milk
Reality: Color changes are usually normal or indicate foremilk/hindmilk imbalance
Myth 3: Fussy babies need formula instead of breast milk
Reality: Fussiness often resolves with dietary adjustments or time
Myth 4: Breast milk allergies are common
Reality: True breast milk protein allergies are virtually non-existent
Forums and Discussion Boards on Babies Reacting to Breast Milk
Many parents have found themselves wondering if their baby could be allergic to breast milk after noticing concerning symptoms like rashes, gas, blood in stool, or fussiness.
While true breast milk allergies are medically impossible, these real-life experiences reveal how food proteins (like dairy or soy) in a breastfeeding mother’s diet can pass into her milk and trigger reactions in sensitive babies.
Popular Forums and Communities:
“My baby started having mucus and blood in his stool…”
“I was EBF [exclusively breastfeeding], and everything seemed fine… until my baby started having mucus and blood in his stool around 6 weeks old. Our doctor suspected a dairy protein sensitivity. I cut out all dairy from my diet, and the blood disappeared after 5 days. It was definitely a wake-up call that what I eat affects my milk — and my baby.”
www.reddit.com/r/breastfeedingI thought she was allergic to my milk…”
“My daughter had such bad reflux and eczema that I seriously thought she was allergic to my breast milk. I was ready to quit. But my doctor said to try eliminating dairy first. I didn’t realize cheese or even trace amounts in bread could cause this. After 10 days dairy-free, she was like a new baby.”
www.whattoexpect.com“Green poop, gas, constant crying — then I cut out dairy…”
“My son had green poop, gas, and was crying after every feed. We were told to wait it out, but someone on BabyCenter mentioned cow’s milk protein allergy. I removed dairy from my diet and saw improvements within days. He started sleeping better, and his poop went back to normal. Never knew breast milk could carry that much of what I ate.”
www.babycenter.com“Cutting out dairy changed everything…”
“Our infant had colic, eczema, and diarrhea — and we were totally lost. I found a thread here where someone described the exact same symptoms, and it turned out to be dairy in her diet. I went dairy-free for two weeks, and sure enough, our baby’s rash faded and he cried way less. I’m still breastfeeding, just more carefully now.”
www.thebump.com
NOTE: Remember that babies can’t be allergic to breast milk itself. It’s usually something in your diet that needs a little tweaking, not the milk your body produces so lovingly.
When to Switch from Breastfeeding (If Ever)
Stop breastfeeding for allergies when the baby has persistent bloody stools, fails to gain weight, or severe eczema doesn’t improve after 4-6 weeks of elimination diets.
Consider switching when multiple food eliminations fail and the baby continues suffering from severe dehydration, constant discomfort, or when mom’s health deteriorates.
Switching should only happen under medical supervision after trying extensively hydrolyzed formulas first.
Formula vs breast milk for allergic babies decisions require careful medical evaluation and shouldn’t be made independently.
NOTE: Always trust your parental instincts – if something seems off with your baby, don’t hesitate to reach out to your healthcare provider for guidance and peace of mind.
Wrapping It Up
Breast milk allergy concerns affect many new parents, but it’s essential to remember that true allergies to human milk don’t exist.
Most infant feeding issues stem from food proteins in mom’s diet, not the milk itself.
With proper identification of triggers, dietary adjustments, and medical guidance, you can continue providing the best nutrition for your baby.
Don’t let allergy fears stop you from breastfeeding. Most symptoms resolve with simple changes, such as eliminating dairy or soy from your diet.
Trust the process, work with your healthcare team, and remember that breast milk remains the gold standard for infant nutrition.
Ready to become your baby’s nutrition detective? Start that food diary today and unlock the secret to happy, comfortable feeding sessions!
Click here to browse our full collection of breastfeeding and baby stuff blogs!
Frequently Asked Questions
How Do I Know if My Baby Is Allergic to Breastmilk?
Babies cannot be allergic to breast milk itself – symptoms like rashes, fussiness, or digestive issues are caused by food proteins from your diet passing through the milk.
Could My Breast Milk Be Upsetting My Baby?
Your breast milk isn’t the problem, but the foods you eat (especially dairy, soy, or eggs) can trigger reactions when their proteins enter your milk supply.
What Are Signs of Milk Allergy in Infants?
Common signs include eczema, bloody stools, excessive spitting up, gas, fussiness after feeds, and green, watery diarrhea, usually caused by cow’s milk proteins in the mother’s diet.
What Does Dairy Sensitivity Look Like in Breastfed Babies?
Dairy sensitivity typically presents as mucus or blood in stool, skin rashes, colic-like crying, frequent spit-up, and uncomfortable gas within hours of the mother consuming dairy products.
