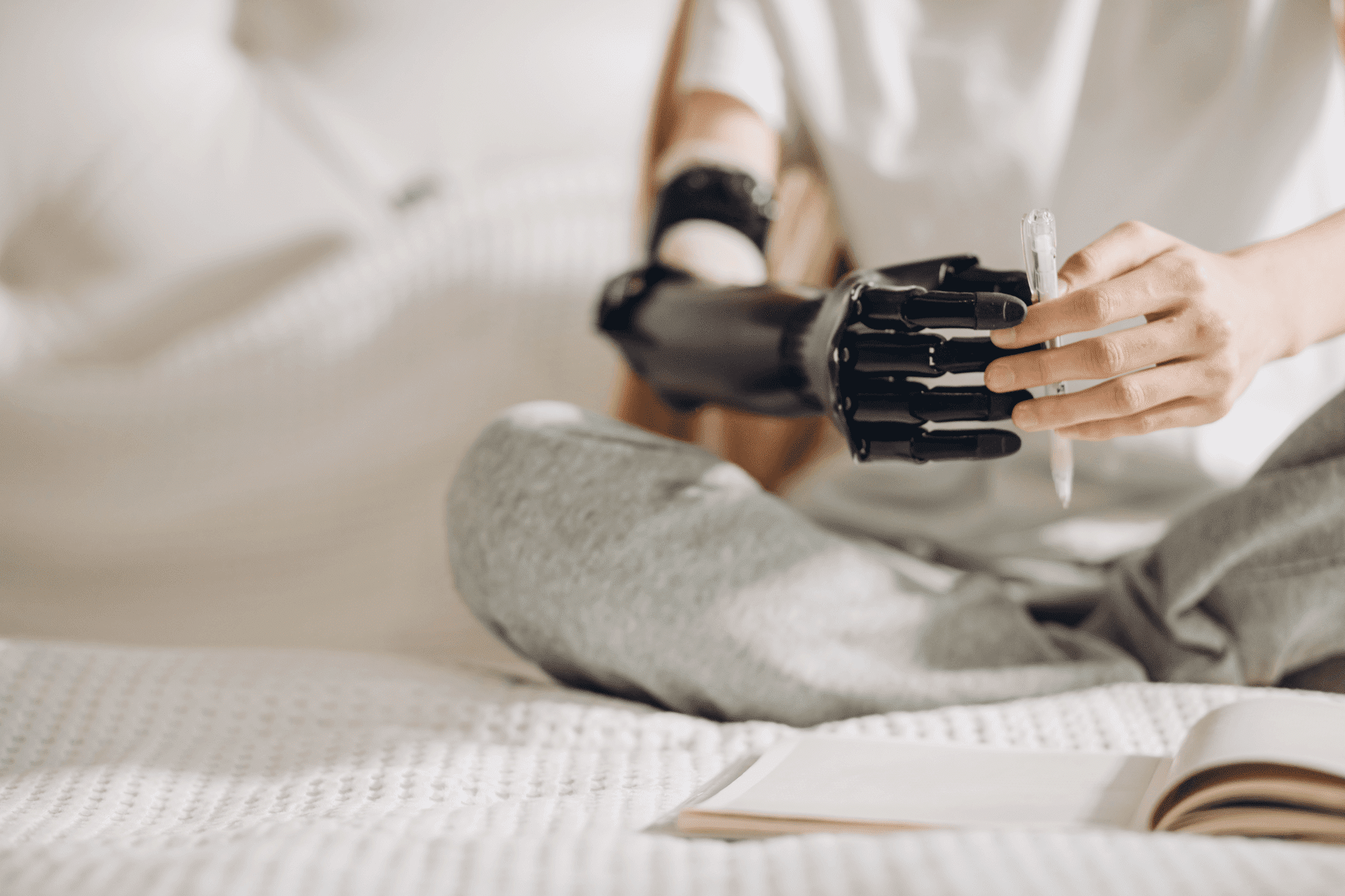
The human hand is a masterwork of biomechanics and a primary tool for interaction, expression, and independence. Its loss is a profound event that challenges not only a person’s physical capabilities but also their sense of self. Wrist disarticulation, an amputation at the wrist joint, preserves the full forearm but presents a unique set of challenges for prosthetics—the retained length can be both a benefit and a liability.
This article will explore the specific functional problems inherent to this level of amputation and demonstrate how modern wrist disarticulation prosthesis systems, with their advanced materials, intuitive controls, and refined design, are now solving them. The journey from overcoming these obstacles is a testament to how human-centered design is transforming the field.
The Unique Functional Challenges of Wrist Disarticulation
Wrist disarticulation presents a paradox for prosthetic design. While the preserved forearm length is a significant advantage over higher-level amputations, it also creates distinct functional problems.
Here are some of the unique functional challenges associated with wrist disarticulation prosthetics:
- Prosthesis Length Discrepancy: The addition of a prosthetic hand and wrist unit often results in a device that is longer than the natural limb, leading to aesthetic and functional issues.
- Cosmetic Mismatch: The length difference can make the prosthesis appear unnatural and hinder activities requiring bilateral symmetry.
- Midline Activity Interference: An overly long prosthesis can obstruct movement for tasks performed close to the body, like dressing or personal hygiene.
- Socket Fit and Suspension Difficulty: The bulbous distal end of a wrist disarticulation stump makes achieving a comfortable, secure, and non-rotating socket fit challenging.
- Skin Integrity Issues: Improperly fitted sockets can lead to discomfort, pressure sores, and skin breakdown.
- Limited Fine Motor Control (Historically): Traditional body-powered systems often struggled to provide the precise, nuanced control needed for intricate hand movements.
The primary challenge is the issue of prosthesis length. Because the amputation occurs at the wrist joint, the residual limb is long. When a prosthetic hand and wrist unit are added, the overall length of the device often exceeds that of the sound hand, creating an aesthetic mismatch and a functional hindrance for tasks performed at the body’s midline, such as getting dressed or reaching into a pocket. Another major hurdle is socket fit and suspension. The distal end of a wrist disarticulation stump is bulbous, a shape that can be challenging to fit comfortably. A socket that is too tight can cause discomfort and skin irritation, while one that is too loose will slip or rotate, compromising control.
This specific fitting challenge requires a high degree of customization, similar in complexity to the considerations for a hip disarticulation prosthesis. Additionally, achieving precise, nuanced control of a prosthetic hand has historically been difficult with traditional body-powered systems, limiting a user’s ability to perform fine motor tasks.
Innovations in Socket and Suspension Technology
Modern prosthetic systems have overcome the long-standing fitting challenges of wrist disarticulation through a blend of advanced manufacturing and new materials. The introduction of 3D scanning and additive manufacturing (3D printing) has been a game-changer. These technologies allow prosthetists to capture the exact, unique contours of a residual limb and create a custom socket with a perfect, intimate fit. This personalized approach addresses the discomfort and fit issues caused by the bulbous shape of the forearm, ensuring a secure connection without painful pressure points.
Equally important are the advancements in suspension systems. Modern designs utilize suction, elevated vacuum, and flexible inner sockets to create a lightweight yet incredibly secure connection. These systems often eliminate the need for cumbersome harnesses, which were a common complaint with older prosthetics. The enhanced security and comfort provided by these modern solutions give the user greater freedom of movement and confidence.
This focus on a stable and comfortable interface is a shared principle across prosthetic development; a similar emphasis on suspension is critical for a prosthetic knee, where a secure fit is essential for a stable and efficient gait. These innovations are not just technological; they are fundamentally about improving the daily experience of the user.
The Leap in Control Systems
The most significant strides in modern prosthetic technology lie in the realm of control and dexterity, directly addressing the limitations of older models. Myoelectric systems, which use sensors to read muscle signals, have advanced to provide intuitive control that was once unimaginable.
A user can now think about moving their hand, and the residual limb’s muscles will generate the electrical signals that the prosthetic hand and wrist translate into motion. This allows for proportional control, meaning the force of the grip can be varied to hold a delicate egg or a heavy tool. The complexity of these systems has also been addressed through innovative design.
Here are some pros and cons of these evolving control systems:
Pros:
- Intuitive Control: Myoelectric systems allow for more natural and thought-driven control compared to traditional body-powered prosthetics.
- Proportional Control: Users can vary the force of their grip, enabling manipulation of both delicate and heavy objects.
- Enhanced Dexterity: Advanced systems and multi-articulating hands allow for a wider range of movements and fine motor tasks.
- Reduced Physical Strain: Less reliance on gross body movements to operate the prosthesis.
Cons:
- Cost and Accessibility: High-tech myoelectric and pattern recognition systems can be very expensive, limiting access for many.
- Training Requirements: Users often require extensive therapy and training to master the nuances of these advanced control systems.
This technology enables a user to perform complex, multi-directional movements, like rotating the wrist and closing the hand simultaneously, with a level of fluidity that was previously impossible. This has fundamentally transformed a user’s ability to perform complex, two-handed tasks, from operating a keyboard to cooking in the kitchen.
Comparing Functional Goals with Lower Limb Systems
While upper and lower limb prosthetics both aim to restore function, their core objectives and the challenges they solve are fundamentally different. For a prosthetic knee or a dynamic response foot, the primary goal is to facilitate an efficient, stable, and energy-conscious gait. The focus is on weight bearing, shock absorption, and propulsion to enable a person to walk, run, or climb with confidence. The engineering challenge is to replicate the smooth, rhythmic motion of a leg.
In contrast, an upper limb prosthesis, particularly for a wrist disarticulation, must solve for a completely different set of problems: dexterity, grip strength, and the ability to manipulate objects with precision. The complexity lies not in replicating a simple hinge joint but in recreating the intricate, multifaceted movements of a human hand and wrist. This is a task that requires an entirely different approach to control systems and component design.
For example, a high-level lower limb amputation, such as a hip disarticulation prosthesis, shares the difficulty of a complex socket interface and significant functional loss.
However, the solutions—a high-tech, microprocessor-controlled joint—are tailored to the unique biomechanics of ambulation. Despite their different objectives, the underlying principles of modern prosthetic development remain the same: customization, advanced materials, and intuitive control are paramount to restoring a high quality of life.
Conclusion
Modern prosthetic systems have effectively overcome the unique functional challenges of wrist disarticulation. By moving past the limitations of older, cumbersome designs, they now offer solutions for fit, length, and, most importantly, control. The use of advanced manufacturing techniques like 3D printing has revolutionized the comfort and security of the socket, while myoelectric and bionic systems have given users an unprecedented level of dexterity.
The parallel advancements in lower limb systems, such as the prosthetic knee, show that a shared philosophy of customization and innovation is at the heart of the entire field. The progress in this area is a testament to the power of human ingenuity, which is continuously striving to create solutions that not only replace a lost limb but also restore a person’s ability to live, work, and interact with their world in a way that feels complete.

