
Finding blood in your baby’s stool can be frightening, but most cases stem from minor issues that resolve quickly. However, specific symptoms demand immediate attention.
Understanding the difference between harmless causes and severe conditions helps you respond appropriately.
This blog covers what blood in stool looks like, common causes, and when to seek help. Sometimes what looks alarming holds a simple answer, but knowing when to act fast makes all the difference.
Disclaimer: This content is for informational purposes only and does not replace professional medical advice. Always consult your pediatrician for proper diagnosis and treatment of your baby’s health concerns.
What Does Blood in Baby Stool Look Like?
Blood in a baby’s stool can appear in various forms depending on its source and how long it’s been in the digestive system. Recognizing the different types helps determine urgency and potential causes.
- Bright red streaks or spots indicate fresh blood, often from the lower digestive tract or minor tears.
- Dark red, maroon, or black tarry stools suggest digested blood from higher in the digestive system.
- Blood mixed with mucus may appear as pink-tinged or bloody streaks in a slimy substance.
Blood location provides important clues; surface blood typically indicates a different issue than blood mixed throughout the stool, helping identify the source more accurately.
NOTE: Foods that mimic blood include beets, tomatoes, red food coloring, and certain medications that can create false alarms.
Common Causes of Blood in a Baby’s Stool
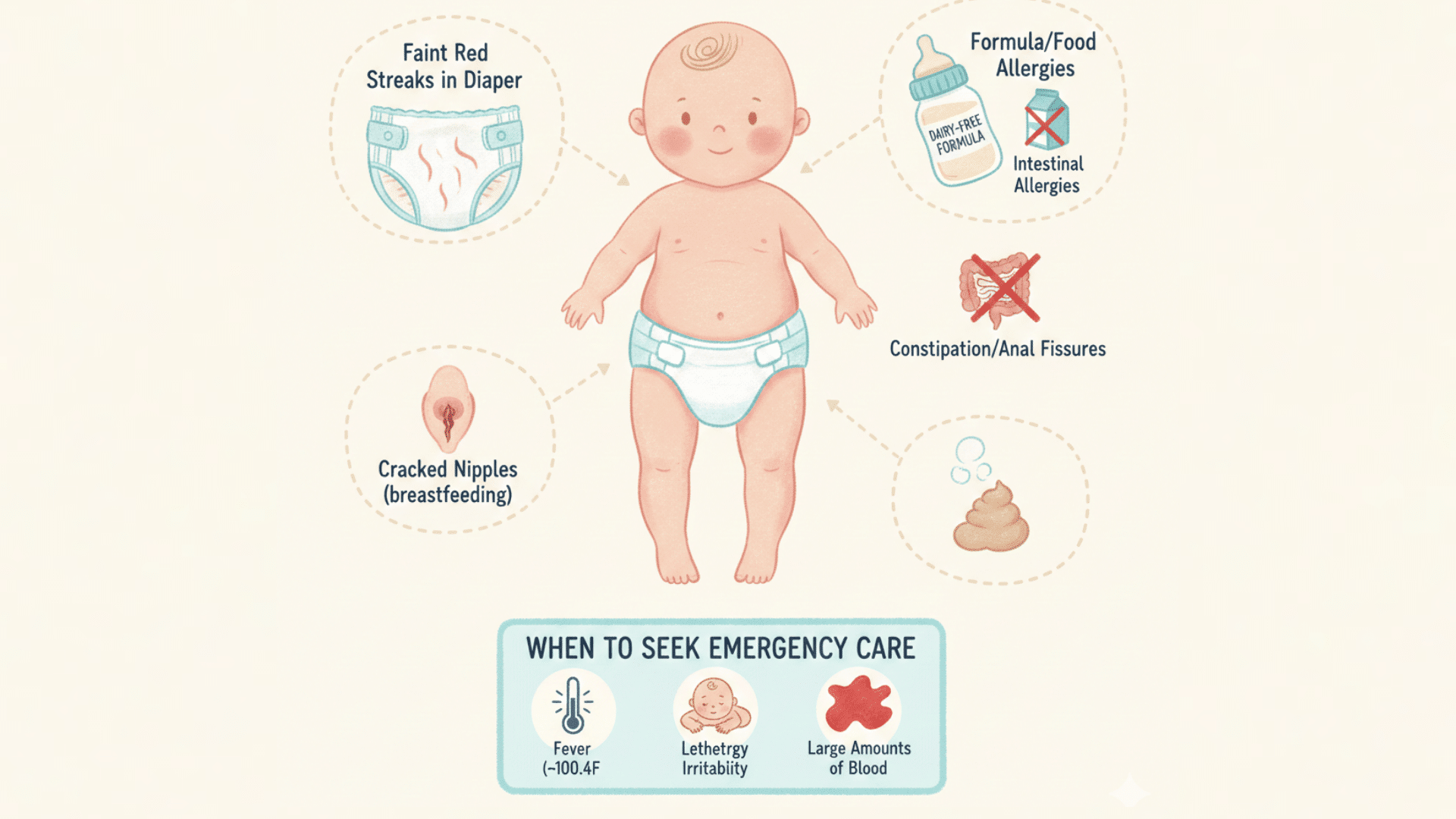
Most cases of blood in a baby’s stool stem from benign causes that resolve with simple treatment or time. Understanding these common conditions helps parents distinguish between minor issues and situations requiring medical attention.
1. Anal Fissures
Anal fissures are tiny tears in the delicate skin around the anus caused by passing hard or large stools, appearing as bright red blood on the surface of the stool or wipes.
These fissures typically heal on their own within days to weeks and are considered the primary cause of blood in infant stool by most pediatricians.
2. Cow’s Milk Protein Allergy (CMPA)
CMPA is the most common food allergy in infants, affecting both formula-fed and breastfed babies with symptoms including blood-tinged mucus in stools, excessive fussiness, vomiting, and digestive discomfort.
Treatment requires eliminating dairy from the nursing mother’s diet or switching to a hypoallergenic formula, as cow’s milk proteins pass through breast milk to breastfed babies.
3. Other Food Allergies and Sensitivities
Babies can develop less common food allergies to soy protein, eggs, or corn, which manifest as infantile allergic proctocolitis, causing inflammation in the colon and rectum.
Despite bloody stools, affected babies typically remain happy, gain weight usually, and recover within weeks once the trigger food is identified and eliminated.
4. Maternal Blood
Breastfeeding mothers with cracked or bleeding nipples may inadvertently pass small amounts of blood to their baby during nursing, which appears harmlessly as faint streaks in the stool.
This benign condition, often overlooked but common in early breastfeeding weeks, resolves once the mother’s nipples heal with proper latch correction and care.
5. Swallowed Blood from Other Sources
Babies may swallow blood from non-digestive sources like nosebleeds or circumcision healing, which then passes through the digestive tract and appears in stool, mimicking a gastrointestinal problem.
The key distinction is that affected babies show no signs of digestive distress, and the blood disappears once the original bleeding source heals.
6. Constipation
Hard, difficult-to-pass stools force babies to strain excessively, leading to anal fissures and visible blood that creates a painful cycle where babies begin withholding stool.
This withholding worsens constipation and increases bleeding, but treating the underlying constipation through diet changes, hydration, or gentle remedies breaks this cycle.
Serious Causes That Require Immediate Medical Attention
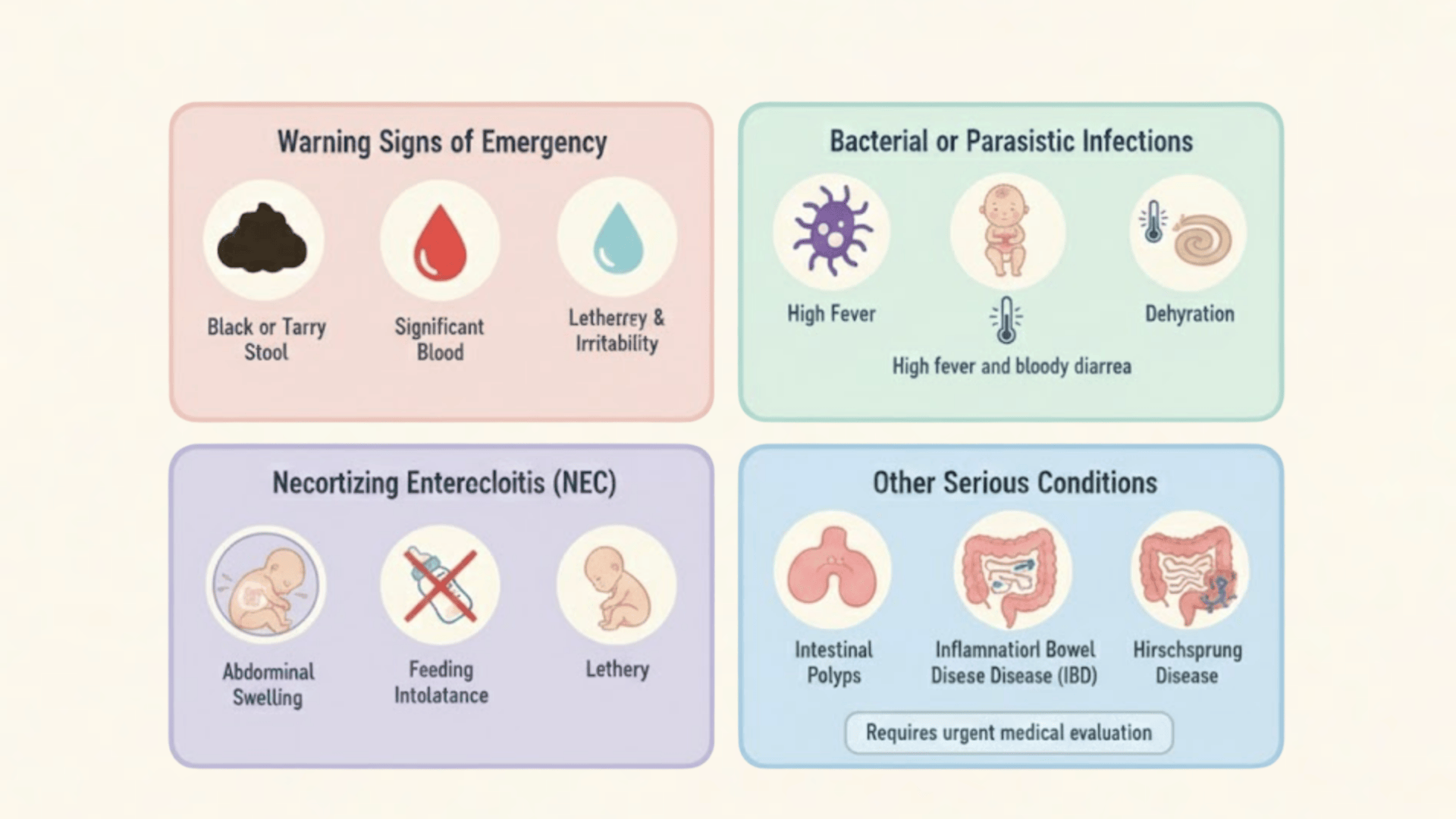
While most blood in a baby’s stool is harmless, certain conditions demand urgent medical evaluation and treatment. Recognizing these warning signs can be lifesaving and prevent serious complications.
1. Warning Signs of Emergency
Black or tarry stools, large amounts of bright red blood, bloody diarrhea, or blood with high fever, severe lethargy, or refusal to eat require immediate medical attention.
Contact your pediatrician or visit the emergency room immediately if these appear alongside dehydration signs, pale appearance, or unusual weakness.
2. Bacterial or Parasitic Infections
Bacterial infections like Salmonella, E. coli, or Shigella cause bloody diarrhea with high fever, severe irritability, and abdominal pain, typically occurring through contaminated food, water, or daycare contact.
Babies are particularly vulnerable to dangerous dehydration from these infections, requiring prompt medical treatment with antibiotics and careful hydration monitoring for recovery.
3. Necrotizing Enterocolitis (NEC)
NEC is a life-threatening intestinal condition most commonly affecting premature babies, involving severe inflammation and tissue death in portions of the intestine.
Symptoms include bloody stools, abdominal distension, feeding intolerance, lethargy, and temperature instability, requiring immediate hospitalization, potential surgery, and intensive medical intervention to prevent fatal complications.
4. Other Rare but Serious Conditions
Rare severe conditions include intestinal polyps causing painless rectal bleeding, inflammatory bowel diseases causing chronic bloody diarrhea, intussusception (intestine telescoping causing severe pain and currant jelly-like stools), and Hirschsprung disease affecting colon nerves.
All require prompt medical evaluation and treatment, ranging from surgical removal to emergency intervention.
When to Call the Doctor vs. When to Go to ER
Knowing when to involve your pediatrician versus heading straight to the ER depends on the amount of blood and how sick your baby seems. Mild, first-time symptoms usually go to the doctor; severe or worsening signs go to the ER.
| SYMPTOM (COMBINED) | CALL DOCTOR | GO TO THE ER |
|---|---|---|
| Small amount of bright blood, baby acting normal, no fever | Yes | No |
| First or second occurrence of blood | Yes | No |
| Large amount of blood OR black/tarry stool | No | Yes |
| Bloody diarrhea | No | Yes |
| Refusing food/drink OR dehydration signs | No | Yes |
| Fever above 100.4°F | No | Yes |
| Severe belly pain, lethargy, or unusual sleepiness | No | Yes |
| Vomiting with blood in the stool | No | Yes |
What to Expect at the Doctor’s Office?
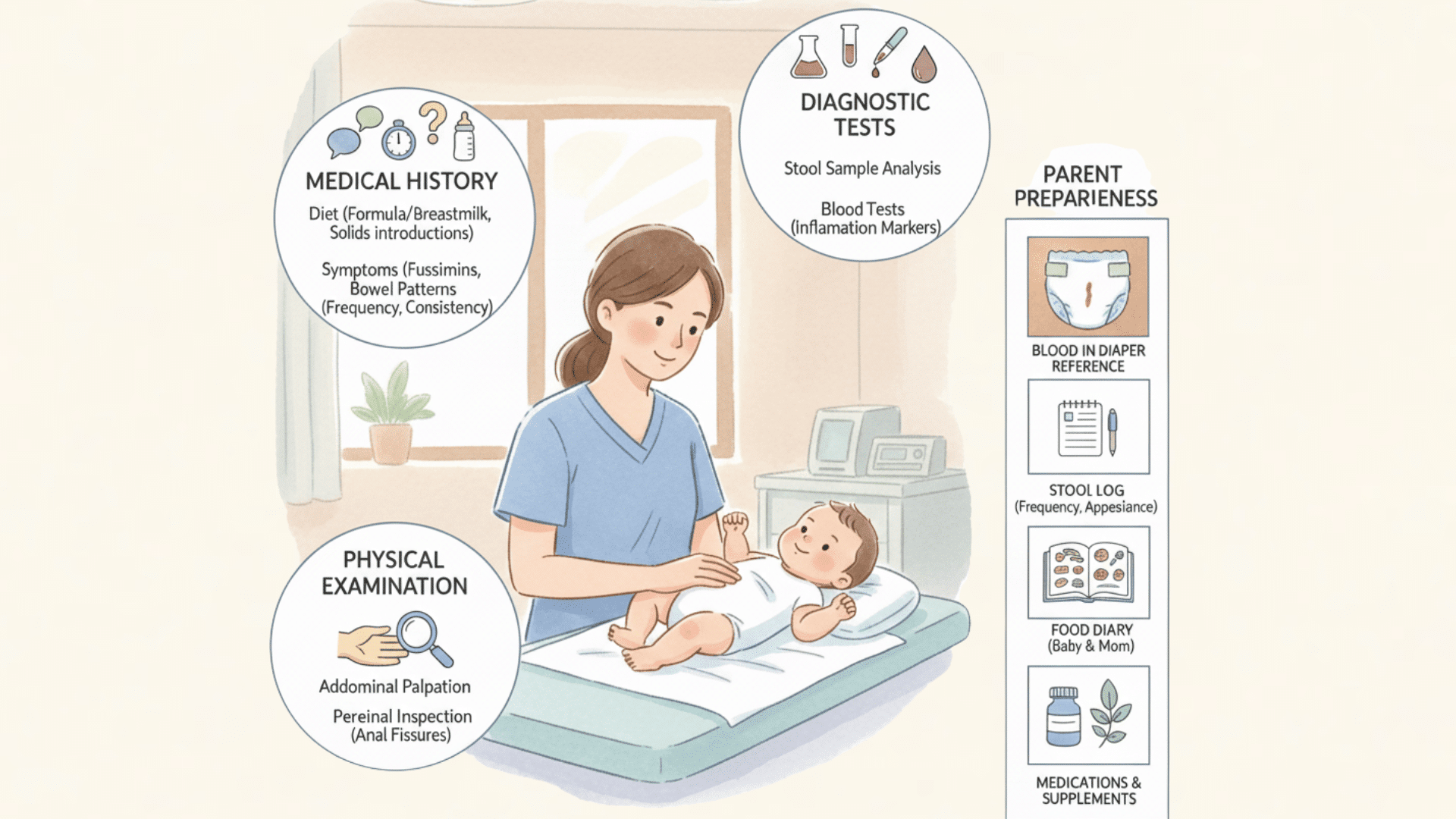
Your pediatrician will conduct a thorough evaluation to determine the cause of blood in your baby’s stool and rule out severe conditions. Being prepared with detailed information helps ensure an accurate diagnosis and appropriate treatment plan.
- Medical history questions include duration of bleeding, blood color and amount, your baby’s diet (breast milk, formula, solids), recent dietary changes, other symptoms, bowel movement patterns, and overall behavior.
- Physical examination involves checking your baby’s abdomen for tenderness, examining the anal area for fissures, assessing hydration status, and evaluating general health and growth.
- Diagnostic tests may include stool sample analysis to check for blood, infections, or allergies, blood tests if anemia or infection is suspected, and, rarely, imaging or endoscopy for serious concerns.
- Bring documentation such as photos of bloody stools, the actual diaper if possible, a tracking log of frequency and appearance, and a complete food diary, including your diet if breastfeeding.
- List all medications and supplements for both the baby and the breastfeeding mother, as certain substances can affect stool color or contribute to digestive issues.
Treatment Options Based on Cause
Most cases clear once the underlying issue is identified and treated. Care may involve skin protection, diet changes, or medical support.
| CAUSE | TREATEMENT | IMPROVEMENT |
|---|---|---|
| Anal fissures | Clean the area, use petroleum jelly, and manage constipation | Days to 2 weeks |
| Food allergies | Remove trigger foods, use hypoallergenic formula | 2 to 4 weeks |
| Constipation | Increase fluids, offer prune or pear juice | Often within days |
| Cracked nipples | Improve latch, use lanolin, air dry | Few days |
| Infections | Antibiotics, hydration support | Varies by severity |
Home Care Tips While Monitoring
While waiting for medical guidance or during treatment, keep your baby comfortable and track symptoms carefully to help identify patterns. These home care measures support healing and provide valuable information for your pediatrician.
- Keep baby comfortable with gentle diaper changes using lukewarm water instead of wipes if the area is irritated, apply barrier cream or petroleum jelly after each change, and change diapers frequently to minimize irritation.
- Prevent constipation through adequate hydration for older babies, age-appropriate dietary adjustments, gentle tummy massage in clockwise circles, and bicycle leg exercises to stimulate bowel movements.
- Establish a routine with consistent feeding schedules and regular opportunities for bowel movements, helping your baby’s digestive system function predictably and reducing straining.
- Track symptoms meticulously by keeping a detailed diary of bowel movements, including blood appearance and amount, feeding patterns, new foods introduced, and any other symptoms like fussiness or fever
- Document what helps or worsens the condition, noting which remedies provide relief, foods that seem problematic, and any changes in stool consistency to share with your pediatrician.
Prevention Strategies
Taking proactive steps to support your baby’s digestive health can significantly reduce the likelihood of blood in stool. These preventive measures address the most common causes and promote overall wellness.
- Prevent constipation by ensuring adequate hydration, adding age-appropriate fiber, and responding promptly to your baby’s poop cues.
- Reduce allergy risk through exclusive breastfeeding when possible, proper formula selection, and introducing solids around six months
- Support breastfeeding mothers by maintaining a balanced diet, staying hydrated, and monitoring potential allergens in your diet.
- Practice proper feeding techniques, including correct bottle positioning, ensuring adequate latch, and burping the baby regularly to reduce gas.
- Schedule regular pediatric check-ups to monitor development, discuss digestive concerns early, and receive age-appropriate nutrition guidance.
Wrapping It Up
Blood in a baby’s stool often resolves with simple interventions like treating constipation or adjusting the diet. Most causes are benign and require only monitoring and basic home care.
Trust your instincts; if your baby shows signs like fever, lethargy, or heavy bleeding, seek medical care immediately.
Keep detailed records and communicate openly with your pediatrician. Remember, you’re your baby’s best advocate. When in doubt, contact your pediatrician today.

